Hospital-acquired infections affect approximately one in every thirty-one U.S. healthcare patients--a statistic that may be profoundly affected by the ongoing COVID-19 pandemic.

The Potential Impact of COVID-19 on Hospital-Acquired Infections
Prior to the SARS-CoV-2 pandemic, HAI's were a serious issue plaguing U.S. healthcare facilities, affecting one in every thirty-one patients, resulting in more than six hundred thousand hospitalizations and seventy thousand deaths in a single year.
According to the National and State Healthcare-Associated Infections Progress Report HAI Hospital Prevalence Survey:
On any given day, about 1 in 31 hospital patients has at least one healthcare-associated infection.
Patients in the 2015 HAI Hospital Prevalence survey were at least 16% less likely than patients in the 2011 survey to have an HAI.
3% of hospitalized patients in the 2015 survey had one or more HAI.
There were an estimated 687,000 HAIs in U.S. acute care hospitals in 2015. About 72,000 hospital patients with HAIs died during their hospitalizations.
However, as a result of the outbreak, concerns are mounting that HAIs may increase due to several factors, including:
- The diversion of traditional infection prevention resources and personal protective equipment.
- Supply chain issues.
- The use of multiple invasive medical devices.
- Prolonged ICU stays, and;
- The increased use of antibiotics to combat possible bacterial co-infections.
According to a recent paper published by the Cambridge University Press;
The full impact of the COVID-19 pandemic on health systems and traditional HAIs remains to be determined.
Significant infection prevention resource diversion is occurring to help manage the outbreak at the health-system level, which will predictably impact HAI surveillance and prevention efforts.
The CMS has recognized the challenges facing the infection prevention community and have suspended penalties associated with the HAC program temporarily.
Other quality programs should consider similar measures.
Now more than ever, health systems should continue investing in their infection prevention programs (both infrastructure and personnel) beyond the current pandemic.
Impact of COVID-19 on traditional healthcare-associated infection prevention efforts
Infection Control and HAI Prevention Strategies
Two primary factors in infection control and prevention strategies are hand hygiene and environmental cleaning and disinfection.
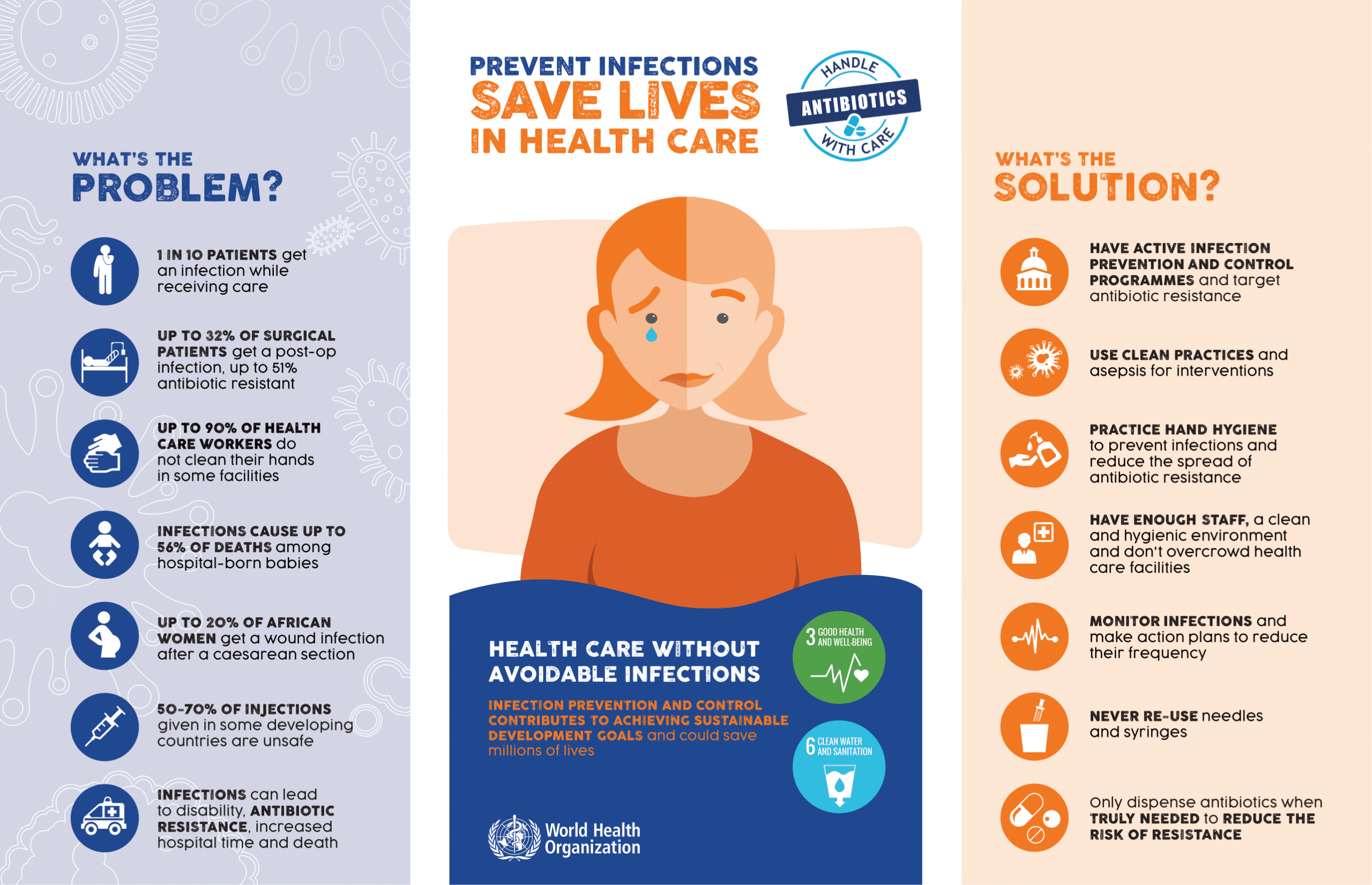
Hand hygiene compliance, even among healthcare workers, was abysmal before the COVID-19 outbreak.
Further, the time allotted for disinfecting surgery and patient rooms has been historically inadequate, resulting in numerous surfaces contaminated with deadly bacteria, some of which are antibiotic and treatment-resistant.
The concern is that the redirection of vital resources from conventional duties to address COVID-19 has left the door open for increased infection.
Now, more than ever, mundane cleaning and disinfection strategies are necessary to combat the spread of illness and protect patient health.
In addition to equipment, partition, bed, and bedding cleaning services, the following is recommended daily or as often as needed:
- Floorcare services - Recent studies have shown that germs, including SARS-CoV-2, are trafficked into a facility on the bottom of shoes and spread through a building via air ducts and dirty hands.
- Basic facility cleaning services - Pathogens and bacteria are found everywhere throughout patient rooms, including restrooms, so they should be scrubbed with microfiber and a commercial-grade detergent before and after each patient visit and as needed throughout the day.
- Touchpoint disinfection services - HAIs are commonly spread via high touchpoint germ hotspots, which should be wiped down several times per day in accordance with foot traffic in and out of the surgery or patient room, as well as other areas throughout the healthcare facility.
References & Resources
- Infection Inside Out: Focus on Hospital-Acquired Infections
- Reduce Risk from Surfaces
- Preventing Healthcare-associated Infections
Takeaway
Prior to the pandemic, HAIs were an enormous challenge for the U.S. healthcare industry, claiming tens of thousands of lives each year.
However, documented progress had been made in the reduction of many of the worst kinds of HAIs, including C.diff and MRSA.
Unfortunately, due to the massive shift of resources to address the ongoing challenge of SARS-CoV-2, patients have been put at an increased risk for secondary infections.
According to the WHO and CDC, basic cleaning and infection prevention and control strategies that involve routine surface cleaning, touchpoint disinfection, and high levels of hand hygiene compliance can combat the spread of secondary bacterial infections.
However, the provisioning of cleaning service personnel may be an issue, which can be overcome via outsourcing for both routine cleaning and day porter services.
Outsourcing to a highly trained and dedicated service provider is a proven method for ensuring the highest cleanliness and safety standards.
Contact us today and discover why Vanguard Cleaning Systems® is the Standard of Clean® for businesses throughout Northwest Arkansas, Missouri, and Oklahoma.
In Oklahoma, dial 918-960-4450
In Arkansas, dial 479-717-2410
In Missouri, dial 417-812-9777
